Introduction
Diabetes is a chronic health condition that affects millions of people worldwide. It occurs when the body cannot effectively regulate blood sugar levels due to issues with insulin production or function. If left unmanaged, diabetes can lead to severe complications, including cardiovascular diseases, kidney failure, nerve damage, and vision loss. Given its prevalence and impact, understanding diabetes mellitus is crucial for prevention, early detection, and effective management.
Diabetes mellitus is characterized by high blood sugar levels, which occur due to the body’s inability to produce or use insulin properly. Insulin, a hormone produced by the pancreas, plays a vital role in transporting glucose from the bloodstream into the body’s cells for energy. When this process is disrupted, glucose builds up in the blood, leading to various health complications.
In this comprehensive blog, we will explore what causes diabetes, the signs of diabetes, and the two main types of diabetes—Type 1 and Type 2 diabetes. Understanding these aspects can help individuals take proactive steps toward prevention and better management of the condition. Whether you have diabetes, are at risk, or simply want to learn more, this guide will provide you with valuable insights into diabetes mellitus and its effects on overall health.
Section 1: What is Diabetes Mellitus?
Definition and Impact on Blood Sugar Levels
Diabetes mellitus is a metabolic disorder that affects how the body processes glucose. Glucose is the primary source of energy for cells, and insulin is responsible for regulating its levels in the blood. When insulin production or function is impaired, glucose cannot be efficiently absorbed, resulting in hyperglycemia (high blood sugar levels).
Role of Insulin and Glucose Metabolism
The pancreas produces insulin to help glucose enter cells. In a healthy individual, insulin ensures that blood sugar levels remain stable. However, in diabetes mellitus, the body’s ability to produce or respond to insulin is compromised. This results in an imbalance that can cause long-term damage to vital organs, including the heart, kidneys, nerves, and eyes.
Diabetes Mellitus vs. Diabetes Insipidus
Although both conditions share the term “diabetes,” they are distinct disorders. Diabetes mellitus relates to high blood sugar levels due to insulin dysfunction, whereas diabetes insipidus is a rare condition affecting the kidneys’ ability to regulate fluid balance. Diabetes insipidus leads to excessive thirst and urination, but it does not involve insulin resistance or high blood sugar levels.
Section 2: What Causes Diabetes?
Understanding what causes diabetes is essential for prevention and management. Multiple factors contribute to the development of diabetes mellitus, including genetics, lifestyle choices, medical conditions, autoimmune reactions, and environmental influences.
Genetic Factors
A family history of diabetes increases the risk of developing the condition. If a parent or sibling has diabetes mellitus, the likelihood of inheriting the condition is significantly higher. Genetic predisposition plays a crucial role, especially in Type 2 diabetes.
Lifestyle Factors
Unhealthy lifestyle choices, such as poor diet, physical inactivity, and obesity, are major contributors to Type 2 diabetes. High consumption of processed foods, sugary beverages, and refined carbohydrates leads to insulin resistance, where the body’s cells become less responsive to insulin.
Medical Conditions
Certain medical conditions, including polycystic ovary syndrome (PCOS), pancreatitis, and hormonal imbalances, can increase the risk of diabetes. These conditions affect insulin production and utilization, leading to glucose imbalances.
Autoimmune Causes
Type 1 diabetes is an autoimmune disease where the immune system mistakenly attacks insulin-producing beta cells in the pancreas. This leads to little or no insulin production, requiring lifelong insulin therapy.
Environmental Triggers
Stress, viral infections, and exposure to toxins have been linked to the development of diabetes. These factors can trigger autoimmune responses or contribute to insulin resistance.
Section 3: Signs of Diabetes
Recognizing the signs of diabetes is crucial for early diagnosis and management. The symptoms can vary depending on the type of diabetes and its severity.
Common Symptoms
- Increased Thirst and Frequent Urination: High blood sugar levels cause the kidneys to remove excess glucose through urine, leading to dehydration.
- Unexplained Weight Loss or Gain: Sudden weight loss is a sign of Type 1 diabetes, whereas weight gain is more common in Type 2 diabetes.
- Fatigue and Weakness: Insufficient glucose in the cells results in low energy levels.
- Blurred Vision: High blood sugar affects the eye’s lens, leading to vision problems.
- Slow Healing of Wounds: Poor circulation and nerve damage impair the healing process.
- Frequent Infections: Diabetes weakens the immune system, making infections more common.
Signs Differentiating Type 1 and Type 2 Diabetes
- Type 1 Diabetes: Rapid onset, insulin dependence, usually diagnosed in childhood.
- Type 2 Diabetes: Gradual progression, insulin resistance, often linked to obesity and lifestyle factors.
Section 4: Type 1 Diabetes vs. Type 2 Diabetes
Type 1 Diabetes
- Autoimmune disorder that destroys insulin-producing cells.
- Common in children and young adults.
- Requires insulin therapy for survival.
- Risk factors include genetics and environmental triggers.
Type 2 Diabetes
- Develops due to insulin resistance.
- More common in adults but rising among younger populations.
- Linked to obesity, poor diet, and sedentary lifestyle.
- Managed through lifestyle changes and medication.
Section 5: Diagnosis and Tests for Diabetes
Common Diagnostic Tests
- Fasting Blood Sugar (FBS) Test: Measures blood sugar after an overnight fast.
- HbA1c Test: Assesses average blood sugar levels over three months.
- Oral Glucose Tolerance Test (OGTT): Evaluates the body’s response to sugar intake.
- Random Blood Sugar Test: Measures glucose levels at any time of the day.
- Continuous Glucose Monitoring (CGM): Tracks blood sugar trends in real time.
Section 6: Management and Treatment of Diabetes
Lifestyle Modifications
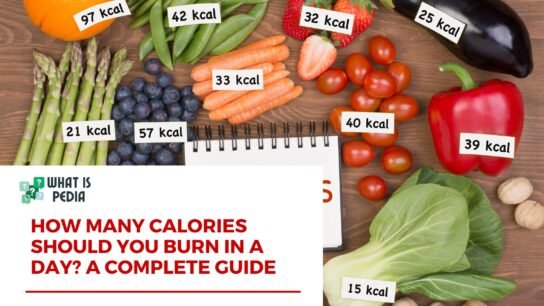
- Healthy Diet: Emphasizing low-carb, high-fiber foods.
- Regular Exercise: Physical activity improves insulin sensitivity.
- Weight Management: Maintaining a healthy weight reduces diabetes risk.
Medical Treatments
- Type 1 Diabetes: Insulin therapy and monitoring.
- Type 2 Diabetes: Medications like Metformin, insulin (if necessary).
- New Advances: Insulin pumps, artificial pancreas, and stem cell research.
Conclusion
Diabetes mellitus is a serious yet manageable condition. Recognizing what causes diabetes and the signs of diabetes can lead to early diagnosis and effective intervention. Both Type 1 and Type 2 diabetes require proper management through lifestyle changes and medical treatment. Prevention strategies, such as maintaining a healthy diet and staying physically active, can significantly reduce the risk of developing diabetes.
Ongoing research continues to improve diabetes treatment options, offering hope for better outcomes in the future. By raising awareness and promoting education about diabetes mellitus, we can work towards a healthier, diabetes-free future.
Read More: What Causes Hearing Loss? Understanding the Symptoms, Types, and Treatment Options